Acute Nephritic Sydrome
Posgt streptococcal
glomerulonephritis
Acute glomerulonephritis
ETIOLOGY
:
Inflammatory complex :
1.
Infection by streptococcal beta-hemolatic
2.
Complex Ag-Ab attack of basement menbrane
3.
Toxin effect of streptococcal to
basement membranous glomerula.
PATHOPHYSIOLOGY
:
karksÞH
enA Glomerula eday Complex Ag-Ab eFVIeGay
-
Inflammmation ( Hematuria , proteinuria )
-
Bi)akeRcaH ( Edema ,
Oliguria )
-
Hypertesion
(Increase afferent artery pressure )
CLINICAL SIGNS
·
Post
Streptococcal infetion of pharynx
-
Fever
-
Sore
throat
-
Malaise
-
Abdomonal
Pain
·
Acute glomerular
inflammation
-
Sudden
onset 1-7 days
-
Oliguria (
Urine < 400ml / day prognosis to acute renal failure )
-
Edema
-
Proteinuria
non selective and hematuria
-
Hypeertesion
PARACLINC
·
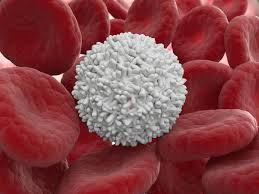
CBC
·
BUN (Blood
Urea-Nitrogen )
·
ASLO
positive
·
Urinalysis
-
Proteinuria
non selective
-
Erythrocyte
cast
-
Leukocyturia
-
Hyaline ,
glanular
·
3
Serologic markers
-
Serum C3
level
-
Anti
glomerula basement membrane antibody (
AGBM antibody )
-
Anti
nucleo cytoplasmic antibody ( ANC antibody )
·
Renal
ultrasonography
·
Renal
biopsy
COMPLICATION
·
Anemia
·
Hyperkalemia
·
Acute
renal failure
·
Chronic
renal failure evolution to ESRD
DIFFERENTIAL
DIAGNOSIS
·
Nephrotic
syndrome
·
Henoch
Schonlein purpura ( Rheumatiod purpura )
·
Lupus
nephritis
·
Berger’s
disease ( Ig A nephropathy )
·
Wegener’s
Granulomatosis : Vasculitis
associated with
-
Glomerulonephritis
-
Resporatory
symptom : Cough , dyspnea , chronic sinusitis , otitis media , hemoptysis .
-
Neuropathy
, purpura , arthritis , scleritis
-
Conformed
diagnosis : C_ANCA , large nodular by chest x-ray , hematuric , and biopsy .
-
Treat by
corticoide or cyclosporine and cotrimoxazole
MANAGEMENT
1. Supporting diet and vitamin B
2. Edema and hyperkaliema Furosemide 1mg / kg
/ dose
3. Hypertesion ( Calcium channel blocker )
4. Antibiotherapy
Ceftriaxone
100mg / kg / day
5. Follow up every month
, ASLO test ?
Extrancilline 2.4 millions / month
References
Current essentials of medicine
MERCK MANUAL , medicine information